
On the Road to Recovery – Using Comprehensive Healthcare Event Reporting to Reduce Medical Errors
In March 2019, a Tennessee woman filed suit against Nashville-based Vanderbilt University Medical Center, claiming surgeons operated on her wrong kidney. As a result, the patient had to have a second surgery to correct the mistake, and she now needs dialysis for life. While this case was both rare and extreme, the fact remains that damaging medical errors are quite common, yet often preventable.
The World Health Organization (WHO) says more than 1 million patients die every year from surgical complications. And, there is a 1 in 300 chance of a patient being harmed during health care.
Clearly, more should be done to improve healthcare safety and quality and reduce risks to patients. Yet to say that the challenges of healthcare risk management are complex would be an understatement. Existing processes for risk management are fragmented and lack standardization. Many healthcare providers continue to use inferior systems that fail to analyze and synthesize data in a meaningful way. And all this in a rapid-fire environment, where threats can materialize in an instant.
Searching for the How and Why
When viewed as an individual benchmark, medical error reports only uncover so much. For example, an incident report of the Vanderbilt case would certainly show that the wrong site was operated on. But the more important question is Why? Perhaps the surgeon had been working too many consecutive hours. Maybe there was misinformation between departments. Or maybe a critical pre-op step, such as marking the operation site on the body, was overlooked. And if it was, why?
The how and why behind an incident are the real agents of change.
Finding the root causes behind errors in patient care is critical if we hope to prevent them from happening again. In fact, the only good that can come of such mistakes is the opportunity to learn from them and make process improvements – ultimately improving the standard of care and saving lives.
Risk Management Software for Increased Patient Safety
Reducing errors in patient care is not about having more medical knowledge, it’s about operational performance. And a basic incident report won’t change much.
When a safety event occurs, the first step is to record the basic facts in a patient’s medical record. While this step is both necessary and required, it excludes the information that is most important for analysis, learning, and operational change in the organization.
When things go wrong, both front line staff and healthcare administrators need access to comprehensive facts and circumstances surrounding the incident – as well as a clear, streamlined, and accountable improvement process. Fortunately, the right performance improvement platform can both identify and offer cues towards effective corrective and preventative actions, or CAPAs.
Hospitals, regional clinics, and surgery centers will benefit greatly from a single, comprehensive system for risk management., particularly one that integrates the many performance measures across the board, and that integrates all these activities into a goal-oriented, coherent whole. In order to keep up with the pace of care, they need analysis and synthesis of data in real-time. And most importantly, they need clear and manageable action plans based on that analysis.
The right platform for quality-safety improvement can provide insight into past incidents, identify existing performance trends, and offer a view of the future. ActionCue CI’s comprehensive dashboard facilitates the collection of information and circumstances surrounding healthcare incidents including planning errors, process errors, and failures to act.
Here are some of the key ways ActionCue CI makes quality-safety tracking and improvement more effective:
- Anyone on staff can originate an Event Report with little or no training
- There are 26 categories of events covered including Complaints/Grievances, HIPAA incidents, Abuse, Plant/Facility, Readmission, Sentinel Events, Security and Work-related Injury
- The distributed workflow not only distributes the workload but obtains inputs from the best people to do so, including those nearest to the time and place of the event
- Event Reports are passed to the next person in the workflow based on roles, permissions and assigned parts of the organization
- The workflow, appearance and experience are designed with expertise in several disciplines
- Individuals or groups have assigned responsibility for each step, but others can observe and review the content, or can be requested to confer on the content
- Workflow progress is tracked so that stalled reports are identified to managers who can send reminders
- Content (documents, photos, videos)can be uploaded/attached to the Event Report at any stage
- Alerts can be immediately sent to select individuals when content of designatedcriteria is saved
- Those with permission can track, review and research the Event Reports using a range of content filters while they are in progress or after completion
- Follow-up activities, beyond the primary track of the Event Report workflow, can be tracked in terms of scheduled reminders and information or documents exchanged, with any internal or external organization
- Built-in analytics and reports provide distribution data (histograms) of content occurrences, weighted analyses, time spent by workflow stage and event category, and much more insight, as soonas the events Reports are finalized, without any time delay or human effort.
- Certain facts and circumstances are tallied in the Event Reports to form data points used in numerous Performance Measures like Fall Rate, Medication Variance Severity, and many more
- Event Reports can be linked to Performance Improvement Action Plans, and vice versa, for easy human analysis
While some of these features may be of particular interest or importance to various users, the real power of ActionCue CI is that it was designed for a specific purpose – facilitating all stakeholders having a fundamentally different relationship with the data that allows them to better leverage their time and energy for true improvement. While the change-averse may initially balk at such a dramatic shift, it is the right approach for long-term gains throughout the organization. Optimal gains can only be achieved through a platform designed for this purpose.
Mistakes in healthcare have bad consequences for everyone, from injured patients to physicians who may face legal and professional troubles. By working to eliminate medical missteps, healthcare professionals can protect patients and themselves while lowering operational and cost inefficiencies in delivering better care. But if institutional practices do not change, nothing will change.

Losing Focus on Value in Value-Based Purchasing
When it comes to discussions about healthcare reimbursement and costs, “Value-Based Purchasing” is a term that gets thrown around quite a bit these days. In fact, many experts say it’s going to be the future for healthcare organizations.
Due to its growing use in hospitals and regional clinics, Value-Based Purchasing (VBP) has become a buzzword in healthcare. But as often happens with buzzwords, the original meaning becomes less salient to most people than their feelings and experiences with the subject. What exactly is the goal of value-based purchasing?
The Goal of Value-Based Purchasing
On paper, the methodology of VBP is simple: pay providers for quality and value, not just volume. Hold healthcare organizations accountable for both the quality and cost of the care they deliver and reward the best-performing providers.
The goal of VBP is to facilitate a high-level of care that is both safe and efficient. To reduce medical errors, lower the rate of accidents, achieve better patient outcomes, and maximize financial rewards. In an ideal world, clinics and hospitals will operate at optimal effectiveness and efficiency – resulting in lower prices for both patient and payor.
The Reality of Value-Based Purchasing
Organizations work hard, month after month, to achieve this noble “value proposition”. But the everyday reality of succeeding for their organization in a Value-Based Purchasing program is far from simple.
Value-based care goals come with their own elaborate set of rules, metrics, benchmarks, reimbursement adjustment tables, and a million other things. The delay between capturing data and applying benchmarks to a provider’s reimbursement is significant. It’s all too easy for care providers to become immersed in the administrative minutiae of VBP and lose track of the program’s highest goal – better value for patients.
Therefore, whether you’re a front-line staffer or a top-level executive, it’s important to circle back to one basic question: “Does what we’re doing truly improve value?”. If the answer is “No” or, (as is often the case), unclear – then it’s time to evaluate the effectiveness of the task, process or tool on a fundamental level.
Getting Back to the Value in VBP
In order to shift the focus back to “value” in a value-based purchasing system, major changes need to occur in how departments think and work together.
Of course, a VBP-participating provider organization cannot completely ignore the necessary mechanics of the program without losing the reimbursement boosts it can provide. However, when the staff and management can focus on actual performance across the majority of their care-delivery operation, on a real-time basis, VBP success becomes a byproduct of genuinely improved clinical performance across the board.
As we see it, there are some real opportunities for core value improvement in the fundamental way the quality improvement operation is executed. For example:
- Change the focus from reporting to insight, learning, and change. Lengthy and detailed reports do not improve anything. Make the improvement process the primary core function, make it effective and efficient, and reverse engineer the way the capture, processing, communication, and work on that related information is built to optimize improvement in Quality and Safety.
- Involve executives by giving them the right lens on the subject matter. ActionCue’s event reports capture the facts and circumstances surrounding each adverse event, while the performance measures and analytics capture a big, coherent picture of the operations. Only by replacing the “too many moving parts” nature of Quality-safety with a complete story can we hope to provide proper executive buy-in and leaders to improve evidence-based outcomes and quality measures.
- Get away from paper as inputs or outputs. Paper is static information that takes human effort to move, change and work on. ActionCue CI gives uses a workbench to support information work and receive actionable insights in a dynamic way.
- Don’t be afraid to re-invent the process. Stop throwing more human effort at things that aren’t getting results, just because it’s “the way we’ve always done it.” That includes classes and meetings, that soon fade and impact the work far less than equipping the staff to actually work differently.
- Think outside the box. The “mandated” way is not always the best way! Don’t let a mandated task, step or artifact chain the organization to an outdated, suboptimal overall process. Look for new and fundamentally more efficient processes that serve goal attainment, even if those small mandated tasks, that deliver less value, seem redundant.
Remember, the most precious things your team produces in running your operation and delivering care are actionable insights to improving value. If you’re working more and getting less of that, CHANGE. Because the goal, after all, is value. Value for patients and value for care providers.
Intuitive Tools for Better Patient Care
Healthcare has too many moving parts. It’s a common cry in the industry, especially for healthcare quality and safety professionals.
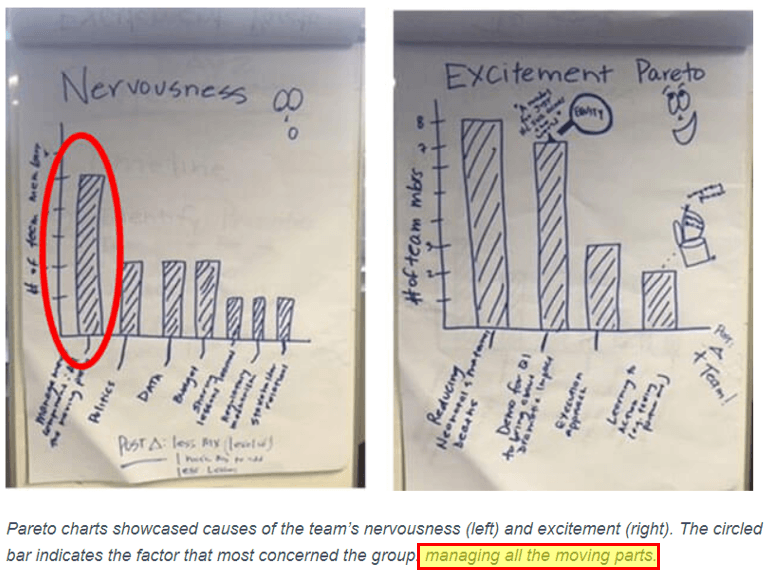
In January 2019, the Institute for Healthcare Improvement (IHI) polled a group of members embarking on a large-scale project to reduce maternal and newborn mortality. When asked what aspects of the project made them most nervous and what made them most excited, “managing all the moving parts” was the top cause of concern.
As the poll indicates, between reporting, forms, metrics and insurance, plus the innate complexities of patient care – things can get complicated very quickly.
The Challenge: Too Many Moving Parts
The “moving parts” dilemma is all too familiar to healthcare quality and safety professionals. When it comes to patient care and process improvement, it’s always been a delicate balance between quality, safety, and context.
Too often, there exists a large gap between “ticking the box” and the actual process of conceiving, planning and evaluating improvements. When metrics and event reporting become mutually exclusive tasks within healthcare organizations, everyone suffers. Departments miss out on the benefit of shared information, and the level of patient care remains stagnant or worse, declines.
There are a few healthcare IT products on the market that aim to tackle the moving parts problem – but most of them fall short. You find yourself manually moving and processing data or repeating tasks because system modules don’t “talk to each other”. Simple calculations are left to the user. Navigation of the application is overly complex and language unintuitive. Users’ engagement with the various systems and methodologically-driven manual processes is daunting and painful.
Healthcare organizations are looking for the most efficient ways to leverage human, financial, and physical resources in support of top-notch patient care. Despite best efforts though, non-universal systems & software, and information silos between departments often get in the way of progress. The result is a lot of fractured effort and reduced productivity.
The Solution: Informed Insights, Action Plans
What if you could spend less time managing “moving parts” and more time providing and improving patient care?
What hospitals need most are healthcare technologies that not only collect data, but also provide context and insights that lead to better and safer patient experiences. They need software solutions that are easy-to-use, intuitive, collaborative and, most of all, coherent.
Quality performance metrics matter, but they don’t tell the whole story. Metrics force you to work with simple data, while what you really need are the actionable insights derived from that data. And, managers and executives trying to drive improvement need answers to “How did we get here ?” and “What are we doing to fix this ?” without going on a safari or waiting on an analyst or staffer to chase and manufacture those answers.
Our number one goal behind the design of ActionCue CI was smoothly bringing together all those “moving parts”. Separate functions and departments for Quality Management, Event Reporting and Performance improvement don’t reflect, and don’t contribute well to, the true, unified goal of optimizing patient care and its costs. More than just another set of spreadsheets, event reporting software, and assembled briefing book – metrics, facts and progress tracking are synthesized into valuable insights with corresponding cues. The innovative new technology supports patient-centered care by facilitating management and work for performance improvement projects. One Goal. One Platform. Coherent Insight.

Role-Appropriate Participation for Everyone in the Clinical Realm
How enabled is your team? Does it matter? The answer to the second question is “Yes”. But how do you enable employees at all levels of a healthcare organization to make a positive impact on the quality-safety of patients and participate in performance improvement in meaningful ways? Prista’s ActionCue Clinical Intelligence application was designed so that all users are able to efficiently and intuitively engage with the platform and process to both provide and interpret data in meaningful ways.
Most healthcare IT applications have user administration based on profiles, roles and permissions, and many also associate the user’s roles with specific parts of the organization. These roles should be straightforward and easy to administer, in order to eliminate the frequently seen dependence on billable services from a vendor or additional analysts and specialists within the organization. This means users see only the things relevant to, and used by, themselves and mostly only at the time those functions are likely to be of interest. This makes it much easier to get to and act on exactly what they need, simplifies or shortens everyone’s learning curve, and significantly helps users stay focused on what they engaged with the application to do.
Probably no one benefits from this aspect more than the CEO and other C-level executives. Because of the typical complexity and numerous moving parts of the quality-safety efforts as described above, those at the top of the organization with enterprise-wide responsibilities very often have to choose between detaching themselves from the workings of quality-safety improvement or drowning in the details, because information is too often not collected or presented in a way that lends itself to a reasonable manner and degree of executive oversight. A common compromise is to add data analysts who work on a constant stream of ad hoc research and reporting requests. Not only is that “solution” expensive, but it also adds cycle time and disrupts the evolving pursuit from one answer to the next question as the skilled executive chases insights in a complex, dynamic environment.
An efficient platform must apply technology advances to directly facilitate the enablement and engagement of all users—even busy executives—with the insights and work being accomplished by the entire staff within the platform. ActionCue CI’s performance dashboard presents that big picture, with easy-to-follow links to additional presentations of related data, information and insight. Data hierarchies are designed to match the cognitive pathways of a healthcare leader, providing easily accessible, real-time insight. Whether it is the insights sought, the contribution of content, the user skill level or the cognitive pathway the user undertakes, a successful platform adapts to the user to deliver a productive and enjoyable experience. Implementing technology to facilitate both productivity and performance improvement is one of the most meaningful ways to enable your organization’s team.
This post is part 4 of our 7 Innovation series. Interested in reading more? Download the 7 Innovations that Deliver Strategic Value in Healthcare White Paper

The Value of Actionable Insight in Healthcare Organizations
Have you ever found yourself staring at row after row and column after column of data and asking yourself “What does this MEAN?”? One of the most valuable skills in today’s workforce is an ability to take all of the data that technology allows us to collect and to make sense of it in meaningful and actionable ways. We believe that all aspects of a quality-safety and performance improvement platform should boil down to this. Prista’s ActionCue Clinical Intelligence application consolidates your data and includes built-in reporting tools to provide instant insight into the most impactful issues that need to be addressed. That’s why we call it the Fast Path to Insight.
At Prista, our mission is to help healthcare leaders achieve optimal clinical and operational performance in the most effective, efficient and sustainable means possible. By addressing a wide variety of entrenched inefficiencies, particularly through the diligent application of technology, human behavior and design principles, our ActionCue Clinical Intelligence application helps those leaders find and prioritize their clinical- and financial-related issues, focus on corrective and preventive actions, and build and sustain an improvement in quality-safety culture.
Instead of delivering dead data in the form of reports, the ActionCue application facilitates action in the management of the improvement process by enhancing communication, focus, learning and accountability. The integration of data into useful insight enables staff at all levels of healthcare organizations to focus on quality and safety improvement and creates enormous positive financial impact. Reductions in fall with injury, hospital acquired infections, re-admissions and many other measurable and actionable issues not only avoid punitive revenue reductions in the Pay for Performance model, but these quality of care and patient experience measures are also meaningful messages to drive engagement and goodwill within the communities served by healthcare organizations.
By creating intuitive and user-friendly experiences, through simplifying on-going and required reporting initiatives, ActionCue CI improves results across multiple goal sets, and delivers real-dollar ROI. By managing clinical performance through meaningful dialogue and easily-tracked performance improvement plans, healthcare leaders can become less reactive and more proactive and step up their leadership in an environment in which it is direly needed.
This post is part 3 of our 7 Innovation series. Interested in reading more? Download the 7 Innovations that Deliver Strategic Value in Healthcare White Paper
