Category Archives for Healthcare Quality
Flu, pneumonia deaths exceed epidemic threshold
Becker’s Healthcare reports statistics on a significant rise in influenza and pneumonia deaths, focusing on flu-related death in 10 states: Alabama, Georgia, Kansas, Louisiana, Minnesota, Missouri, New Jersey, Oklahoma, South Carolina and Tennessee.
With such outcomes, the tracking of clinical staff immunizations, according to guidelines, becomes critical to impact the outcomes as well as for compliance reasons. As with many standards, being compliant needs at least as much focus by healthcare management as reporting compliance. How well is your healthcare delivery organization doing at its part in containing influenza, pneumonia and other diseases through vaccination efforts ?
Our research shows that the most successful vaccination programs have good operational tracking that:
- is particularly easy for capture or entry of vaccination data
- is structured to match the reporting requirements as to demographics and disposition
- provides no-hassle reports that are very accessible, easy to interpret and focused on action for staff, managers and executives
- is institutionalized so everyone is aware and on the same page
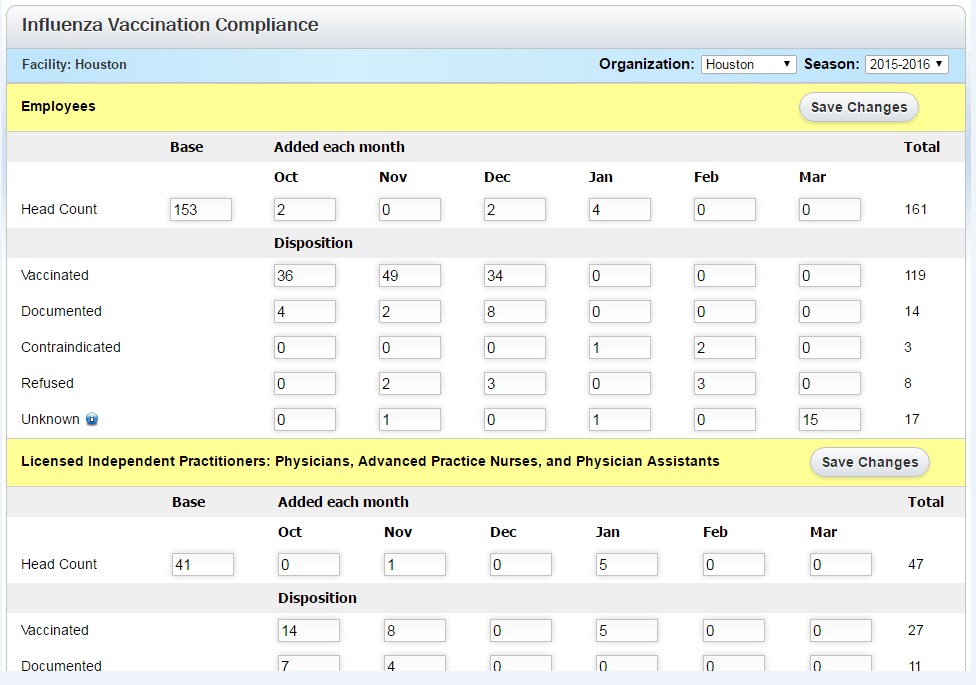
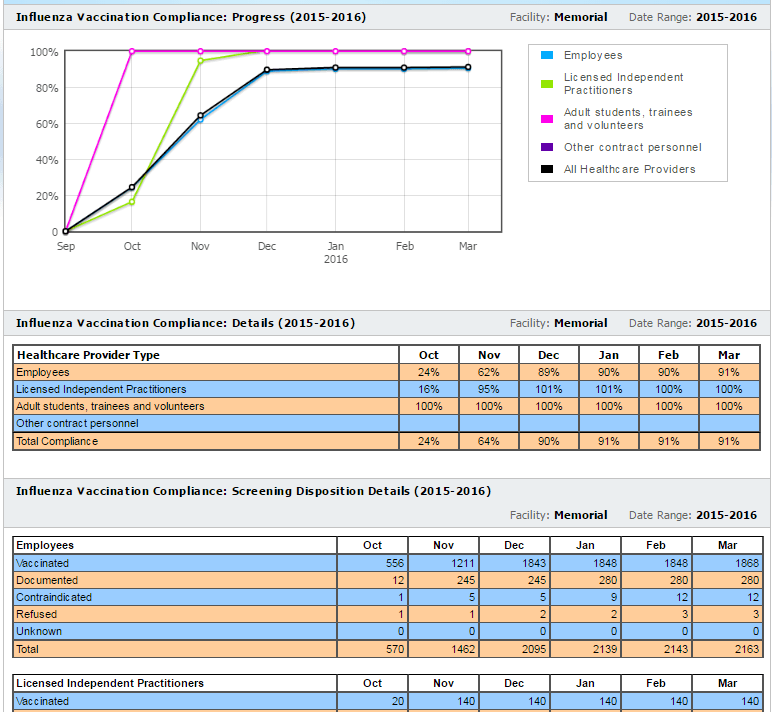
ActionCue Clinical Information has built-in forms for CDC/NHSN-defined data requirements and a built-in report with both detailed data and immediate indication of immunization program effectiveness.
Form for easy entry of disposition data
Built-in Report
ActionCue CI saves clinical managers 20-30% of their work time while delivering more insightful, actionable information across the entire Quality, Patient Safety and Performance Improvement effort. Over 90% of organizations using the ActionCue application are compliant with vaccination requirements and compliance is just that clear.
National Healthcare Quality Week
As a contribution to the celebration of all of those who work diligently and passionately in Healthcare Quality, we would like to plant a seed of thought, an innovative vision, of pursuing the goals of Quality (and its intimate partner, Safety) to get better outcomes, more consistently, while using less effort and cost, and feeling less frustration. In other words, an easier path to improvement.Historically, “Quality” has been tightly associated with “reporting” and it may be understandably difficult for many to separate their thinking in that regard from the collection and manipulation of data, research on and calculation of Performance Measures, visual analysis of number grids and graphs, generating and compiling reports, and sitting though hours of review meetings to share and discuss the information. And much of the effort in Quality reporting targets higher level management and especially external parties, rather than the clinical staff themselves. Many describe such responsibilities as overly mechanical and time-consuming, seriously reducing the time and brain power left over for the cognitive work of imagining, planning and confirming improvement in healthcare delivery. Even highly-respected overt methodologies, which supposedly serve that improvement goal, often add to the mechanical effort requiring procedural education, special forms, jargon, and more meetings.To a great degree, much of that is accepted, personally and organizationally, as being “the Quality job”, but perhaps there is vision of something different. A breakthrough.
The reason we talk about a breakthrough is important. There is a very strong tendency, while trying to improve processes, to simple tweak the same activities and artifacts that have been part of the process for a long time. That is definitely the case with quality. If we focus on the cognitive path, from observation to improvement, and design optimally for the digital/electronic medium to support that, then real progress can be made. This must not be equated to having users take on the mindset, language or skills of “techies”. It should be the case that the power of technology and especially the design expertise that is coupled to it, is delivered into the operative “space” of the targeted users.
When that is done well, much of the mechanics, physical activities and artifacts can be eliminated and the most precious resource of the clinical staff – their professional intellectual capabilities – are channeled toward the improvement goal. To put that in tangible terms, this vision is about one place where all the information involved in the Performance Measures of Quality Management, in Safety Event reporting and investigation, and in the Action Plans for Performance Improvement exist in intuitive, connected, workflows. The net effect is a design that radically reduces both labor and mental exertion to get actionable insights.
Realizing such a vision may be challenging because of departmental, process, policy and political barriers, the natural inhibitors of fear, ego and comfort, and the tyranny of time and money invested in the “old ways”. But why should you or your organization let those stand in the way of your passion to pursue Quality the way you’ve always known it should be done?
Alliance with CIHQ
Prista Corporation and the Center for Improvement in Healthcare Quality (CIHQ) Collaborate to Enhance Patient Safety

About the Collaboration
Prista and CIHQ are driving for the same goal – to radically improve the effectiveness and efficiency of quality-safety* efforts in healthcare delivery organizations. While the organizations differ in services and approach, their philosophies related to providing education, resources and tools to the healthcare community are well aligned.
Through a variety of communication vehicles, CIHQ provides education, shares perspectives on patient safety and compliance, and presents available resources and tools. Through its ActionCue Clinical Intelligence online application, Prista enables subscribers to significantly reduce and streamline the mechanics and manual data manipulation of the improvement processes for quality-safety.
Billie Anne Schoppman, Chief Mission Officer at Prista reflects “CIHQ is innovative, nimble and responsive just like Prista and makes a great partner to really help care providers break through some stasis and inertia to put best practices to work and drive quality and safety improvement like never before – effectively, efficiently and consistently.”
Rick Curtis, Chief Executive Officer of CIHQ, explains his perspective; “We’re excited to partner with Prista. Both our organizations share a common Mission and purpose. Our partnership will enable Prista clients to access our vast array of web-based support services, and our clients will benefit from access to Prista’s innovative quality and patient safety management platform. It’s not just a win/win for both companies, it’s a win/win for our respective clients.”
Be on the lookout for lots of content and opportunities to participate in demonstrations to learn how Prista’s ActionCue platform and CIHQ’s education, advice and content go hand-in-hand to advance our joint subscribers and members to the forefront of America’s healthcare organizations.
* – Quality-safety reflects Prista’s position that care quality and safety for patients are inseparable and should naturally be addressed together in an integrated improvement–centered management process.

About CIHQ
The Center for Improvement in Healthcare Quality (CIHQ) is a membership-based organization comprised of over 300 acute care and critical access hospitals across the United States. Member organizations enjoy a comprehensive program of web-based and other support services designed to help them be successful in their accreditation and certification compliance efforts. CIHQ is also recognized as a deeming-authority by CMS for acute care and long-term acute care hospitals.
About Prista
Prista provides the ActionCue® Clinical Intelligence online application, a very innovative platform integrating Quality Management, Event Reporting and Investigation, and Performance Improvement functionality. Beyond a dashboard or reporting tool, ActionCue provides a complete work environment for staff, management and executives to obtain immediate insights into all clinical issues and what is being done to improve them, to own and drive the improvement-centered quality-safety process as never before.
Interoperability: An EHR Litmus Test
By Don Jarrell
Interoperability has become a watch word in the healthcare business. The need to deploy electronic health record (EHR) systems across the board has put a strong spotlight on the need for different digital healthcare systems to communicate with one another, from doctor’s offices to hospitals to labs to insurers. Right now, they don’t. Perhaps more accurately, they don’t communicate fully and easily.
The interoperability problem is not a new one in the business world, nor is it confined only to the healthcare industry. The financial sector and the oil and gas industry have both succeeded in making complex data sets accessible across different vendors’ systems, so we know it can be done
Most if not all of the coverage given to this issue by the media is focused on the difficulties it presents to the provider-patient-insurer side of healthcare. While this is certainly part of the problem, there is more to the equation. Many companies like ours provide solutions on the operational/quality/safety side of healthcare, and we continually see the effects that lack of EHR interoperability has on the patient quality and care staff with whom we work. Instead of improving operational processes, digital EHR systems create more work. For example:
- Needed data and information must be extracted “by hand” from the EHR and then re-entered, often with human “processing” in between.
- Data that could be useful as care quality indicators is not accessible from the EHR.
- Staff must fill data holes themselves, falling back on the (inefficient) use of spreadsheets and paper.
In short, what is experienced by too many users of EHR systems is akin to the closing scene of Raiders of the Lost Ark – vast storage with little chance of efficient retrieval for useful purpose. Data warehouses are supposed to process all that data into easily-retrievable, value-added information products that serve the needs of users outside the system.
In an interoperable world, hospitals will use all the data available to them, no matter where the data resides, to manage and improve quality, and they will do so efficiently. All their digital systems will have access to discrete data elements and will be able to use this data easily. Equally important, there won’t be a demand for the labor-intensive tasks now required of staff.
For now, while we wait for full interoperability to arrive, the best you can do is be an informed consumer. Understand the interoperability issue, and be wary of sales peoples’ claims about the ability of their product to communicate agnostically. Apply a litmus test to salespersons’ claims by making these key requests:
- Show me how a clinical manager can retrieve clinical care counts like the total number of Patient Days, Foley days, ventilator days, or medication doses administered.
- Show me how a quality manager can retrieve summarized operational and financial data used in quality and clinical performance management, like Cost per Patient Day, Length of Stay variables, and Admission, Discharge and Transfer (ADT) tallies.
- Explain to me how much of the difference between the demonstration and my “day 1” experience with the application comes from customization that takes time and that we must pay for.
At best, lack of interoperability is frustrating. At worst, it can put a hospital at risk. There is a lot of data locked in an EHR system, and much of it could make a significant difference to patient care quality and safety. Applying this litmus test to any EHR system you are evaluating will help identify the system that will best interface with the rest of your digital systems with the data that you need to operate efficiently.
A Culture of Quality: What It Is and What to Break to Get It
By Don Jarrell
Is there a healthcare organization anywhere that doesn’t want to provide top quality care? This is one of the highest priorities among healthcare professionals and hospital managers. It also may seem like an unachievable dream for many. Between staffing limitations, regulatory requirements and inter-department difficulties, many organizations don’t see a clear path to achieving their quality goals.
Providing top quality care and operating/performing efficiently require a certain way of working throughout the organization—a culture of quality. Embedding a culture of quality is a transformative undertaking and often requires big changes to achieve. Said more bluntly, it means breaking a lot of things.
What is a culture of quality? There are five fundamental components.
- An overall perception of quality. This is a subjective view, an opinion, held by staff and management that is rooted in day-to-day experience. It is influenced greatly by the other four components.
- A learning organization. A hospital with a culture of quality is committed to continuous improvement. While errors in patient care are certainly not encouraged, staff members do not play the “blame game” when a mistake does get made. Instead, the organization takes the opportunity to learn from mistakes in order to improve.
- Open, transparent and bi-directional communication. Because a culture of quality is non-punitive, there is no reason to avoid reporting events. There is no such thing as an event that is too insignificant to report—this includes capturing “near misses,” which will contribute to a more complete picture of care status. With this kind of comprehensive information gathering, the organization has a much more complete basis for learning and performance improvement. When errors do get made, feedback is constructive. No one, including management as well as staff, feels that they need to hide information from others or share only with a few individuals or departments. This fosters more robust two-way communication between the organization’s management and the “in the trenches” professionals, which will naturally increase focus on quality.
- Teamwork. A culture of quality is inclusive, both within units and across units. Functional and informational siloes do not exist, and when the need arises individual will cross functional lines to help.
- Management advocacy. A culture of quality exists from the top down. Management from the highest level in the organization and into all operational units are active advocates of the culture. Apologies for the cliché, but they walk the walk and talk the talk—and the commitment to quality moves from a statement on a wall plaque to a statement made by the daily actions of every member of the organization.
How are you doing so far? Does your organization have a check against each one of these components? If not, how can you get there?
To figure out how to create a culture of quality in an organization that lacks one, it is useful to decide what needs breaking. Often, an organization that does not have a culture of quality has the opposite characteristics to those listed above. For example:
- Units are in informational and functional siloes, so there is a “this is not my problem” attitude when crises arise or help is needed elsewhere in the organization.
- Information is hoarded rather than shared, both within and across units.
- Management may talk the talk of quality, but they don’t follow through in day-to-day activities and therefore don’t demonstrate any commitment to it.
- Event go unreported, and the same mistakes keep reoccurring.
A useful way to find what needs breaking is to take the list of characteristics above and turn it on its head. In other words:
- When management are clear and active advocates of quality, teamwork is fostered.
- When teamwork increases within and across units, there is more open and transparent communication.
- When there is more open communication, learning and continuous improvement is enhanced.
- And when this string is in place, there is a clear overall perception of a commitment to quality.
This prompts questions like:
- How can management clearly demonstrate its commitment to quality on a daily basis? The answer might be as simple as the old “management by walking around” strategy—get management out of their office suites and into the units, asking questions and observing activity.
- What will motivate staff to play well with others? Take away the blame game, make it safe for questions to be asked and mistakes to be identified. Foster cooperation by eliminating reasons for hoarding information and resources.
- How can information be made more readily accessible to everyone? Find ways that information can be accessed by anyone, any time, without having to run the gauntlet of authority.
- What will switch us into learning mode? Make that readily accessible information easy to analyze and set up ways to gain deeper insights from it, then act on those insights in order to make improvements.
Figuring out what needs breaking to transform to a culture of quality depends on your own particular environment, but there is one often-overlooked catalyst that will support transformation in any organization. Software that includes the five fundamental components of a culture of quality in its design is invaluable because it promotes a culture change simply through daily use. In other words, incorporate the right software into the right places, and you will see the right changes occur naturally—and sustainably.