In 2014, the Triple Aim proposed by IHI in 2007 became the Quadruple Aim. This transition occurred because the objectives of the Triple Aim – better...
3 Reasons Why “Designed by Clinicians” is Not Going to Save Healthcare IT
A recent article in Medical Economics, “The Promise of Next Generation EHRs” was an interesting read. It got me thinking, and there were a few...
On the Road to Recovery – Using Comprehensive Healthcare Event Reporting to Reduce Medical Errors
In March 2019, a Tennessee woman filed suit against Nashville-based Vanderbilt University Medical Center, claiming surgeons operated on her wrong...
Intuitive Tools for Better Patient Care
Healthcare has too many moving parts. It’s a common cry in the industry, especially for healthcare quality and safety professionals. In January...
Role-Appropriate Participation for Everyone in the Clinical Realm
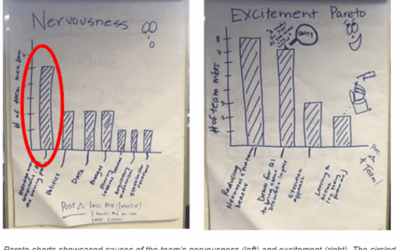
How enabled is your team? Does it matter? The answer to the second question is “Yes”. But how do you enable employees at all levels of a healthcare...
The Value of Actionable Insight in Healthcare Organizations
One of the most valuable skills in today’s workforce is an ability to take all of the data that technology allows us to collect and to make sense of it in meaningful and actionable ways.
Beyond Reporting to Collaborative Management Facilitation
Have healthcare IT tools successfully improved the ability of organizations to provide exceptional patient care? Our application designers, with...
Reducing Preventable Errors Requires a Sustained Shift in Processes and Culture
Preventable medical errors are a serious issue in healthcare and are estimated to be the third leading cause of death in the US, behind cancer and...
Driving Efficiency at All Levels: Organization, User, Provider
Everyone knows time is money, and healthcare consumes too much money. Therefore, it stands to reason that a major objective for hospitals and...