Category Archives for Helping Hospital CEOs
Tackling the Top 10 Patient Safety Concerns with a Culture of Safety – Part 1
The ECRI Institute recently published their Top 10 Patient Safety Concerns for Healthcare Organizations for 2017. Several of these items were on last year’s list, which means we in healthcare still have work to do to drive improvement and meet targeted goals.
Aside from just highlighting new and recurring safety concerns, this list is also a great starting point for inspiring patient safety discussions and setting priorities in your own organization. Here are some ways you can target these concerns by developing a culture of safety.
Let’s begin by counting down, David Letterman style, from ten to one. Since there is much we can say about each finding, we will be covering only 5 safety concerns in this article and the remaining 5 in a second article.
10. Inadequate organization systems or processes to improve safety and quality
There are numerous studies that link error prevention to a culture of safety—being proactive and setting strong preventive strategies rather than waiting for patients to be harmed. This is such an important issue that the Sentinel Event Alert recently addressed the essential role of leadership in developing a safety culture.
Unfortunately, healthcare has been very slow to adopt a culture of safety. Let’s take a look at exactly what a culture of safety is and how leadership is essential to creating one in an organization.
What is a “Culture of Safety”?
Safety cultures have been around a long time, but they’ve only recently been adopted in healthcare. High-reliability organizations are committed to safety by consistently minimizing adverse events at all levels, from frontline providers to managers and executives. This commitment establishes a culture of safety built around the following 7 pillars:
- Leadership
- Teamwork
- Evidence-based
- Communication
- Learning
- Just culture
- Patient-centered
If you’ve been with The Joint Commission and several of the accreditation agencies, you know that leadership has always been first. We kind of take it with a grain of salt, but we can’t anymore. Leadership has to be the most important thing that happens.
The drive needs to start from the top and involve more than executives just putting a stamp on the policy and the plan. Leadership has to own a culture of safety, and when they own it, the team owns it.
Getting real, evidence-based data helps with the communication and the learning of your team members. Leaders have to support a just culture of learning rather than blaming and balance individual accountability with organizational responsibility.
Finally, a culture of safety needs to be patient-centered. You need to include the community and the patients in everything that you do.
9. Management of New Oral Anticoagulants
Tracking adverse events for anticoagulant drugs for has been a part of safety reporting for years, but four new oral anticoagulant medications have been approved since 2014. Here are some strategies and questions you may want to consider when managing these new additions.
Standardized order sets based on individual’s indications
Are you using standardized order sets? Maybe it is time to review to validate if they are evidence-based and individualized.
CDS to alert practitioners to duplication of therapy
Do you have clinical decision systems that can alert your practitioners about duplications or errors in protocols? Having flags on your systems is critical.
Multidisciplinary team plans for reversal of anticoagulant therapy
Consider a multidisciplinary approach to assessing, monitoring and treating for reversal of therapy. Break down the silos that have been around too long.
Reversal agents should be readily accessible
What compliance process measures are you tracking? Are the effective in getting you the information you need to improve? In ActionCue CI, we have a measure for tracking Reversal Agent Usage. This is an example of error prevention, analyze and assess where the problems are and fix it.
Collection and analysis of events
Collection and analysis of events is what ActionCue CI does well. Let’s go one step further and take action for improvement.
8. Inadequate Management of Behavioral Health Issues in Non-Behavioral Health Settings
Behavioral health hospitals have been doing this for quite some time, but healthcare hospitals are not as good at recognizing a patient’s behavioral health. It’s essential that you start preventatively tracking behavior before it becomes a norm in the environment. When you do that, you get outcomes that you can analyze and prioritize.
Your tracking system should include clinical as well as unsafe environment special events. ActionCue CI gives users a Behavior event category training staff to be competent on identifying, reporting and resolving issues. One event ActionCue CI tracks is rapid response. Train your staff now to be competent on identifying those issues, early signs and behavior cues. Don’t wait until it gets to be serious.
7. Opioid Administration and Monitoring in Acute Care
This is a serious situation in this country, not just in acute care. You want to track all of your rescue drug and narcotics usage. But how? Are you looking at narcotic adverse drug events? What’s your reversal drug rate? How many times have you had to use your reversal drugs and for what reasons?
You also need to look at your protocols. What are your protocols for rapid response? Do you have the right equipment? Do you need to buy new equipment? You need to be looking at your medical equipment to make sure it’s up to standards.
Finally, you need to look at the nursing process as you’re investigating events and recommending solutions. You need to go back to look at the basic process so that you’re not forgetting anything as you’re assessing.
6. Patient Identification
Many healthcare settings have stopped tracking patient identification errors. But when you consider that out of 7, 613 events, 9% resulted in patient injury, including two deaths, this is still a serious issue that needs to be addressed from the leadership down.
Leaders can start by fully supporting patient identification initiatives by prioritizing the issue, engaging clinical and nonclinical staff, and asking staff to identify barriers to safe identification practices.
Go back to tracking your patient identification and include in your policies and procedures the contributing causes to the problems the team identified from the event reports. Make this something in your investigation process that your staff are looking at. Your end users are your best value. They’re the ones who see everything that’s going on and who know what needs to be fixed. Give them the opportunity to be involved.
Imagine if you had a button in your event that would automatically create a performance improvement action team. Let’s say the safety risk manager sees that this is the fifth time he’s seen patient identification as a problem. With the click of a button, he decides to create a team. The team works from within the application which serves as a working platform so they can collaborate. Reports are generated automatically, which include the month-to-month analysis and compares agencies and experts that you want to compare yourself to.
The best thing, however, is that you also get the action plan attached to a scorecard report and run chart in ActionCue CI. This is created in real time so you don’t have to wait. It’s all about efficiency. Why should a quality manager go to a committee meeting, decide that she needs a team and spend 2-4 weeks getting one together? She should be able to have the information she needs at her fingertips that she can drill down into.
Focus on the Process
It’s difficult and unsustainable to cram everyone’s head so full of education to the degree that they will continually act in a heroic manner to overcome flaws or deficits in institutional processes and leadership. Until we focus on optimizing the work itself with best process innovations, technology, leadership, goals and respect, organizations will “keep on getting what they’ve always got,” which is not the culture of safety we all need.
In part 2 of this article, we will review the remaining top 5 patient safety concerns for healthcare organizations as they apply to our focus on building a culture of safety.
7 Steps to Increasing ROI with Performance Improvement
For a long time, Quality and Safety Event reporting have been recognized as important but often downplayed tasks when it came to getting the attention of executives and allocating resources. Shifting investments and allocating resources has become even more of a challenge as budgets continue to get tighter and tighter.
Quality-related reimbursement, as applied through Value-Based Purchasing (VBP), MACRO/MIPS, ACO programs and other components in the pay-for performance (P4P) model, have only increased the pressure without providing much guidance on how to actually improve quality.
Although the goal of submitting quality and safety reports and data to external organizations is becoming something more than just checking a “to-do” item off the list, much of the reporting and education efforts in hospitals and other healthcare organizations fall short of making real advancements in Performance Improvement.
The ROI that can perk up executives’ attention and guide their investment is to make Performance Improvement more effective and efficient. While Performance Improvement has been a focus for decades, most organizations focus on the wrong things, such as manually gathering information and data and over-educating staff on the theories and science of QI methodologies. Others are still wasting their time with more meetings, more documents and artifacts and more working overhead.
Worse still, all of these efforts suffer negligible support from innovative IT solutions that are specifically designed to support more efficient and effective Performance Improvement. This is the year, maybe even the quarter, to change that.
Start from the Top
Championing the shift from investing in reporting to investing in the Performance Improvement process itself has to come from the top. Senior management up to the C-suite needs to not only lead, inspire and set the direction, but also provide the resources and fully communicate the importance of creating a smarter and more efficient Performance Improvement process.
Instead of merely asking staff and managers to just “work harder and better,” the goal needs to be about making their job easier and more streamlined.
7 Steps to Better Performance Improvement
An efficient Performance Improvement system needs to be supported by innovative and intuitive IT and can be achieved by taking the following steps.
- Abandon historically-rooted inefficiencies, including artifacts and activities of decades-old QI programs, functional and organizational boundaries that disrupt workflows and manual data gathering and processing.
- Get everyone on the same page with tools that integrate improvement, all quality metrics and event reporting/investigation.
- Ensure every internal reporting and analytic activity drives into improvement.
- Focus on enabling the improvement work correctly instead of over-educating the staff.
- Prioritize synergistic, internal, real improvement activities over external reporting.
- Make sure the access and presentation of needed insight for executives is just right—not too deep and complex nor too shallow and impenetrable—so they can own and drive the effort appropriately.
- Implement a technology-enabled PI workbench specifically for improvement efforts that does all of the above, streamlines and offloads manual efforts from staff and leaders, delivers results and ROI and supports a real culture of improvement in quality and safety.
Improving ROI with Technology
Each of these steps has the potential to be a project in its own right and a daunting task at that. Fortunately, a growing awareness of how Performance Improvement and Quality and Safety reporting can feed one another is prompting a shift in technologies and platforms to support this new focus.
ActionCue CI was built intentionally to increase ROI by changing how Performance Improvement is managed and facilitated using the steps outlined above. Learn more about how ActionCue can help executives, risk/quality managers and clinical staff bring Performance Improvement into the 21st century.
Flu, pneumonia deaths exceed epidemic threshold
Becker’s Healthcare reports statistics on a significant rise in influenza and pneumonia deaths, focusing on flu-related death in 10 states: Alabama, Georgia, Kansas, Louisiana, Minnesota, Missouri, New Jersey, Oklahoma, South Carolina and Tennessee.
With such outcomes, the tracking of clinical staff immunizations, according to guidelines, becomes critical to impact the outcomes as well as for compliance reasons. As with many standards, being compliant needs at least as much focus by healthcare management as reporting compliance. How well is your healthcare delivery organization doing at its part in containing influenza, pneumonia and other diseases through vaccination efforts ?
Our research shows that the most successful vaccination programs have good operational tracking that:
- is particularly easy for capture or entry of vaccination data
- is structured to match the reporting requirements as to demographics and disposition
- provides no-hassle reports that are very accessible, easy to interpret and focused on action for staff, managers and executives
- is institutionalized so everyone is aware and on the same page
ActionCue Clinical Information has built-in forms for CDC/NHSN-defined data requirements and a built-in report with both detailed data and immediate indication of immunization program effectiveness.
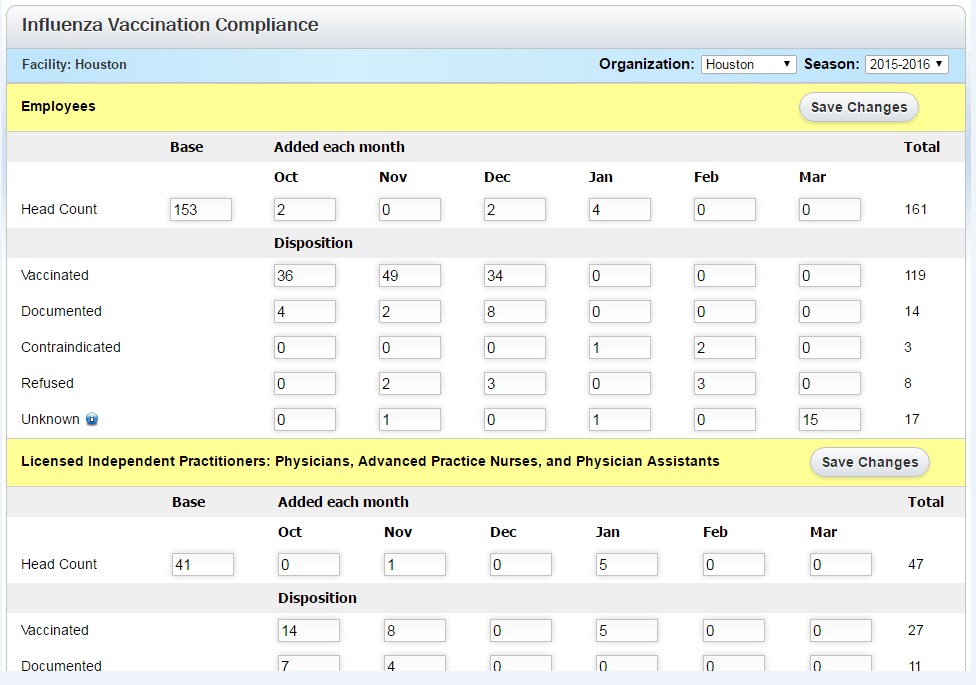
Form for easy entry of disposition data
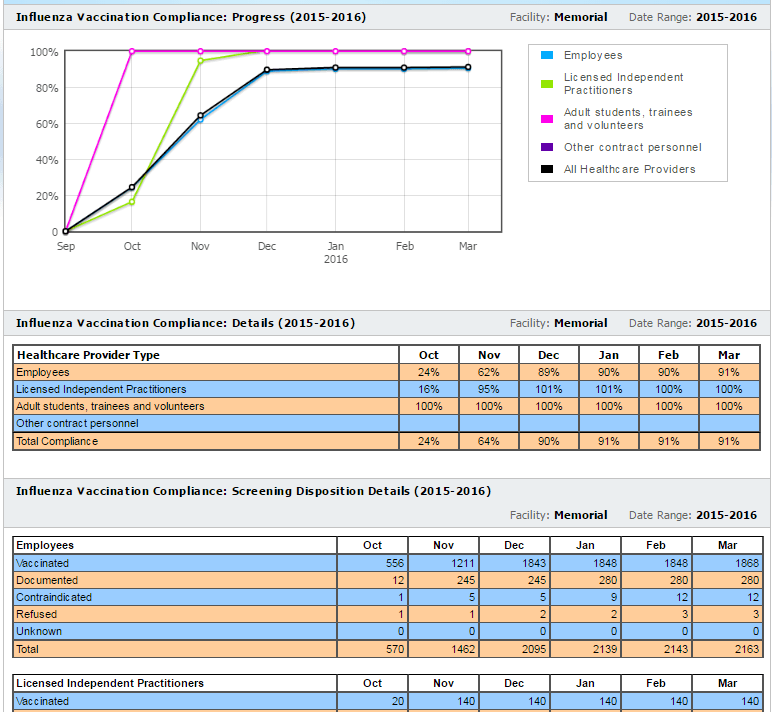
Built-in Report
ActionCue CI saves clinical managers 20-30% of their work time while delivering more insightful, actionable information across the entire Quality, Patient Safety and Performance Improvement effort. Over 90% of organizations using the ActionCue application are compliant with vaccination requirements and compliance is just that clear.
A Culture of Quality: What It Is and What to Break to Get It
By Don Jarrell
Is there a healthcare organization anywhere that doesn’t want to provide top quality care? This is one of the highest priorities among healthcare professionals and hospital managers. It also may seem like an unachievable dream for many. Between staffing limitations, regulatory requirements and inter-department difficulties, many organizations don’t see a clear path to achieving their quality goals.
Providing top quality care and operating/performing efficiently require a certain way of working throughout the organization—a culture of quality. Embedding a culture of quality is a transformative undertaking and often requires big changes to achieve. Said more bluntly, it means breaking a lot of things.
What is a culture of quality? There are five fundamental components.
- An overall perception of quality. This is a subjective view, an opinion, held by staff and management that is rooted in day-to-day experience. It is influenced greatly by the other four components.
- A learning organization. A hospital with a culture of quality is committed to continuous improvement. While errors in patient care are certainly not encouraged, staff members do not play the “blame game” when a mistake does get made. Instead, the organization takes the opportunity to learn from mistakes in order to improve.
- Open, transparent and bi-directional communication. Because a culture of quality is non-punitive, there is no reason to avoid reporting events. There is no such thing as an event that is too insignificant to report—this includes capturing “near misses,” which will contribute to a more complete picture of care status. With this kind of comprehensive information gathering, the organization has a much more complete basis for learning and performance improvement. When errors do get made, feedback is constructive. No one, including management as well as staff, feels that they need to hide information from others or share only with a few individuals or departments. This fosters more robust two-way communication between the organization’s management and the “in the trenches” professionals, which will naturally increase focus on quality.
- Teamwork. A culture of quality is inclusive, both within units and across units. Functional and informational siloes do not exist, and when the need arises individual will cross functional lines to help.
- Management advocacy. A culture of quality exists from the top down. Management from the highest level in the organization and into all operational units are active advocates of the culture. Apologies for the cliché, but they walk the walk and talk the talk—and the commitment to quality moves from a statement on a wall plaque to a statement made by the daily actions of every member of the organization.
How are you doing so far? Does your organization have a check against each one of these components? If not, how can you get there?
To figure out how to create a culture of quality in an organization that lacks one, it is useful to decide what needs breaking. Often, an organization that does not have a culture of quality has the opposite characteristics to those listed above. For example:
- Units are in informational and functional siloes, so there is a “this is not my problem” attitude when crises arise or help is needed elsewhere in the organization.
- Information is hoarded rather than shared, both within and across units.
- Management may talk the talk of quality, but they don’t follow through in day-to-day activities and therefore don’t demonstrate any commitment to it.
- Event go unreported, and the same mistakes keep reoccurring.
A useful way to find what needs breaking is to take the list of characteristics above and turn it on its head. In other words:
- When management are clear and active advocates of quality, teamwork is fostered.
- When teamwork increases within and across units, there is more open and transparent communication.
- When there is more open communication, learning and continuous improvement is enhanced.
- And when this string is in place, there is a clear overall perception of a commitment to quality.
This prompts questions like:
- How can management clearly demonstrate its commitment to quality on a daily basis? The answer might be as simple as the old “management by walking around” strategy—get management out of their office suites and into the units, asking questions and observing activity.
- What will motivate staff to play well with others? Take away the blame game, make it safe for questions to be asked and mistakes to be identified. Foster cooperation by eliminating reasons for hoarding information and resources.
- How can information be made more readily accessible to everyone? Find ways that information can be accessed by anyone, any time, without having to run the gauntlet of authority.
- What will switch us into learning mode? Make that readily accessible information easy to analyze and set up ways to gain deeper insights from it, then act on those insights in order to make improvements.
Figuring out what needs breaking to transform to a culture of quality depends on your own particular environment, but there is one often-overlooked catalyst that will support transformation in any organization. Software that includes the five fundamental components of a culture of quality in its design is invaluable because it promotes a culture change simply through daily use. In other words, incorporate the right software into the right places, and you will see the right changes occur naturally—and sustainably.
Computers vs. Humans: Divide to Succeed
by Don Jarrell
Time after time in our work with hospitals engaged in improving quality and safety management, I have seen management and staff making the same big mistake. They try to do work that they are not suited for, and more often than not end up overwhelmed because of it.
They are doing tasks that their computers should be doing.
When it comes to dealing with all of the information surrounding quality and safety management:
- Computers have perfect memories; humans not so much.
- Computers can store huge amounts of data without forgetting one thing; a human can have a hard time finding the coffee cup they just laid down.
- Computers can analyze reams of data without fatiguing; humans become error-prone after just a short time engaged in this kind of activity.
Said another way:
Computers are good at:
- Capturing
- Storing
- Computing
- Repeating
- Reporting
People are good at:
- Creating
- Solving
- Deciding
- Learning
- Acting
Would you ask a computer to do any of the things that people are good at? I hope not. Forget all the talk about artificial intelligence whirling around these days; the fact is that business computers today are not able to match humans in the creating-solving-deciding-learning-acting space.
And the same is true going the other way. Asking a human to infallibly capture-store-compute-repeat-report on an ongoing basis is very far from effective. In fact, it can be significantly risk-prone. Humans should not be doing the work of computers, just like computers are never expected to do the work of humans.
How does this relate to patient care quality and safety management? Data is being generated 7/24/365. Unless all that data is being captured by a computer set up to do productive things with it, humans are left to make sense of it before they can ever get to the tasks that they are good at. Though they may use computers—in the form of endless spreadsheets—to help them organize and analyze, there is no way a human can match a computer for efficient capture-store-compute-repeat-report tasks. As a result, many quality and safety managers spend too much time dealing with data and not enough time gaining insights for solving, deciding and taking action.
The equation for effectiveness, and for improving quality and safety programs, is appropriate division of labor. Set up the computers to do what they do best so that the humans can do what they do best. Think of the computer as an “intelligence enhancer,” taking on tasks it is suited for and providing rich results that can be used by humans to solve challenges and make improvements.
(Side note: I do have a caveat here. I’ve been saying “computer” throughout, but in reality it’s not the computer so much as the software that makes the difference. You can have two identical computers running different software packages designed to perform the same functions, and end up with widely different results. In order to make the division of labor really work, you must have well-designed software that fits your purpose. I’ll be addressing this topic in a future post.)