Category Archives for Helping Hospital CEOs

Driving Efficiency at All Levels: Organization, User, Provider
Everyone knows time is money, and healthcare consumes too much money. Therefore, it stands to reason that a major objective for hospitals and healthcare systems should be to save time and resources at all levels of the organization and throughout the supply chain. There are several facets to the drive for efficiency, but we’ll focus on the three main levels that successful performance improvement tools can make a positive impact on productivity and cost.
Organization
One way to pass time savings onto organizations is to operate the SaaS model of delivery, in which software is licensed on a subscription basis and is centrally hosted. This eliminates the need for incremental infrastructure—or the maintenance of it—in order to obtain additional benefits. There are several additional benefits in operational cost by not offering the “package and deliver” approach as an option for the customer, as some companies do. A commitment to operating at high levels of efficiency means providers are able to make the acquisition and continued use of the platform remarkably inexpensive.
One of the most impactful ways Prista passes efficiency onto organizations is by reducing the amount of customization utilized within our business model. Although it’s important to be responsive to customers’ needs and requests, the vast majority of healthcare IT customization is based on personal preferences, rather than needs, especially those aimed at imitating paper forms, previous processes, or outdated mandates. The fact is, customization can be a very lucrative business model for vendors and a very large, ongoing expense for customers. This is detailed in our recent blog post “Customization: The Gift That Keeps On Costing.” Aside from the real-dollar costs of significant ongoing customization, there is the added investment of time for key hospital staff and management in creating detailed requirements, reviewing revised software and testing functionality throughout the customization process, not to mention the learning curve of healthcare professionals on the language, disciplines and processes of the software business.
In contrast to the customization-oriented model, successful providers should focus on the turnkey nature of their application. A great deal of healthcare and clinical domain expertise went into the design of the ActionCue CI platform, so that workflow processes, terminology, content selection, and styling are already present “out of the box.” This way, organizational leaders don’t need to spend time specifying what they need or expect in the application. Aside from the healthcare knowledge applied, UI/UX designers should deliver the application to the customer as a finished product useable by the customer within days of start-up, rather than as toolkit that takes six to nine months before the “go live” date.
To accommodate the variability of customer types, including short-term acute hospitals, ambulatory surgical centers, and home health and rehab, and to adapt to the evolution of the quality-safety efforts over time, we made ActionCue CI extremely configurable, so customers, sometimes with the assistance of support staff, can adapt the application, using plain English configuration selections, quickly, efficiently and usually without any cost.
Individual User
The specific design of the application should save time among key users throughout the organization. By ensuring the routine and administrative functions of the application are easy to use and understand, organizations almost never have to hire data analysts or additional clerical staff to assist with workload or technical tasks.
ActionCue CI’s fast, intuitive event reporting reduces the time between an event being reported and getting resolved and allows users to easily and quickly prove they are monitoring quality within the organization. The systems’ workflows were designed to not only match the natural tasks and processes of users, but also shape their behavior by encouraging methodologies that produce targeted results, and increase efficiency and accountability. The design goes beyond ease-of-use to advance the way in which healthcare organizations engage with information in an application.
Using ActionCue, staff can create comprehensive, insightful and simple reports within minutes, which reduces the amount of time executives spend in meetings analyzing confusing or incomplete data sets. At a glance, healthcare professionals can see the real-time condition of their entire facility’s quality and performance initiatives.
Provider
SaaS-model companies, such as Prista, operate on the latest technology platforms, facilitating rapid development and deployment of changes, making them far easier and less expensive to maintain. Companies that have started out as such build their entire operations around utilizing the most up-to-date technologies and methodologies, so their internal operating expenses are lower than those of traditional software companies. These and other efficiencies allow SaaS-model companies to pass their savings along to customers, driving down prices, usually as non-capitalized monthly or annual subscriptions.
Additionally, Prista support staff, with whom customers first and regularly engage, have credentials in Quality Management and Safety. Those staff members also have input on the product design, so that content delivered is accurate, correctly applied, and easy to understand. The ongoing working relationships provide users with a sense of partnership in which they gain knowledge of how the application works, and how it can be best applied to their role.
Efficiency was a guiding principle for the Prista business model, and it’s incorporated into every facet of the ActionCue CI platform. We’re proud to pass our savings along to our customers and ensure ActionCue is driving efficiency at the larger organizational level, as well as making the day-to-day functions of key users more simple and enjoyable. If you’d like to learn more about driving efficiency within your healthcare organization, check out this recent blog post.
This post is part 1 of our 7 Innovation series. Interested in reading more? Download the 7 Innovations that Deliver Strategic Value in Healthcare White Paper

Reverse Engineering an Optimal Performance Improvement Process
In technology circles, reverse engineering is the process of starting with a given end state, such as a product, device, conceived process or operation, and figuring out—in reverse—how to build it. The evolved current state of healthcare quality and performance improvement warrants a similar reverse engineering exercise, and, when executed properly, can result in a truly optimized process, positively impacting patient care and safety.
The Performance Improvement Landscape
Historically, the hospital functions of Quality Management, Safety Reporting and Performance Improvement were predominantly carried out to produce data and documents for submission to external parties, including accreditors, regulators, government agencies, researchers and the like. Those external parties defined the content, format and methodologies of the material to be submitted, and those hospital functions operated toward the objective of sending or submitting the various data and reports in the form and frequency mandated. The actions hospitals took in response to the data and reports was secondary, limited and typically initiated at a much later time than when it was submitted. This delayed, disjointed and reactionary approach proved ineffective for enacting real change within the organization.
Today, with the progressive shift into the system and cultural environment of Pay for Performance, rapid, efficient improvement of clinical outcomes is the internal responsibility of hospital staff all the way up to the C-suite. The game has changed fundamentally, and this priority must remain the focus and goal for hospitals to ensure their success, if not survival.
As described in the Harvard Business Review article, “Why Process is the U.S. Health Care’s Biggest Problem,” processes for medical care and therapies are often localized, personalized and very difficult to improve systematically and fundamentally. These widespread irregularities and weaknesses also apply, maybe even more intensely, to administrative processes, including Quality Management, Safety Event Reporting and Performance Improvement. It is human nature when trying to improve processes to hold on to, and simply shuffle, the artifacts and activities of previous processes, impeding meaningful change. This, too, is admittedly a widespread practice within healthcare administration.
Reverse Engineering for Optimization
For this reverse engineering exercise, we must depart from the activities and artifacts of previous processes built around the different original goal of simply producing reports. With a focus on accomplishing meaningful improvement in quality and safety of patient care, we recognize that the goal is really to optimize a mental pathway to insight that leads to taking corrective action. Those organizations producing the same data, reports, and documents they always have, and trying to accomplish the new goal of active, internal improvement, must undertake a tremendous amount of human effort to cover the distance between the old deliverables, built for an old goal, and the accomplishment of the new goal. Resource constraints, misguided efforts, organizational boundaries, and inadequately designed tools and systems make this ongoing effort a huge problem of ineffectiveness and inefficiency.
While the optimal environment and process for improvement-centered work still involves capturing, processing, analyzing and presenting data and narrative information from the clinical environment, it also requires a relatively advanced design for an integrated, collaborative working platform. The priorities of such a design should center on learning and action for improvement. Technology can be harnessed to bring a wide array of quantitative data, qualitative facts and circumstances of events, assessments of contributing causes and corrective actions from investigations, reference material on procedural innovations and best practices, and tracking of communication and referrals, right to the fingertips of Performance Improvement (PI) experts.
By changing the quality-safety improvement effort of the organization from one of “too many moving parts” to a coherent whole aimed at the comprehensive goal of improved quality-safety for patients, healthcare organizations can finally make real progress on several important fronts. This is a crucial step in the objectives many experts talk about: achieving effective executive leadership and creating/sustaining a culture of quality. In order to exist as a transformative element, delivering real process change, an effective platform must not simply wrangle data, but rather embody communication, teamwork, attention-focusing, prioritization, standardization, and other aspects of management facilitation, guiding individuals and the organization collectively towards a united goal. Only then can clinical performance improvement succeed and serve executives’ strategic clinical, regulatory, and financial objectives.
What are the benefits and pay-offs of having a truly effective and efficient quality-safety improvement process?
With patient care being so fundamental to the organization’s operational, regulatory and financial objectives, a sustained, optimal improvement process has both tactical and strategic impacts, including:
- Clinical staff and executive management enjoy immediately recognizable, significant time-savings within their respective roles in the pursuit of quality-safety, through aggressive leverage of technology, balanced with a pleasant and effective user experience for healthcare professionals. This is increased by a much higher degree of collaboration across the Quality Management (QM), Safety and PI organizations, with those functions being tightly integrated, resulting in greater flexibility in assignment and staffing.
- The organization’s executives’ leadership is better engaged in terms of (1) setting and communicating direction and focus for the improvement goals and efforts, and (2) facilitating proper executive oversight through clear and timely “big picture” views, critical alerts, selective insights into the process and the ability to very easily drill-down to the desired level of detail.
- By centering on the quality-safety improvement process, attention and action are focused on impacting the very elements affecting reimbursement penalties, non-reimbursed care, remedial compliance actions, litigation costs, insurance premiums, and other Pay for Performance and “cost of quality” factors, which take a big bite out of the organization’s top- and bottom-line finances. Effects on real-dollar ROI have been proven repeatedly.
- History has shown that trying to educate staff into a significant change or ramp-up in motivated work effort is typically ineffective or short-lived. However, by upgrading their work from passive, transactional tools, like basic databases and report generators, to advanced workflows designed to carry out best practices, the work itself changes. This transforms their thought processes, and then attitudes and motivation follow and are sustained. It is strongly suggested this is the only way to develop the much-sought “culture of quality”.
- Unifying and simplifying the visibility of all clinical performance issues – as opposed to everyone’s being overwhelmed by the countless, fractured elements – has a collateral benefit of keeping the whole team alert and focused on those things on which they should be working. This collective mindset helps the organization be more proactive than reactive, more disciplined than frantic, and more cooperative than competitive or fault-finding.
This is the kind of innovation you’ve been searching for and can now obtain. By reverse-engineering the performance improvement process, healthcare organizations can part with ineffective and outdated processes, and invest in improvement-centered solutions that go beyond simply producing reports for external parties, and instead use insights to drive action that improves the quality and safety of patient care.

Bouncing Back from a Hospital Safety Penalty
In December of last year, the federal government penalized 751 hospitals for having high numbers of patient injuries, retroactively reducing their Medicare payments by 1% for each patient’s stay, as well as reducing the amount of money the hospitals receive to teach medical residents and care for low-income individuals. These reductions will continue until the end of the government’s fiscal year in September of 2018. The harsh reality of reductions for those listed hospitals, and the potential financial and operational impacts on other hospitals in the future, serve as a call for action among hospital leaders.
The penalties are controversial. Many in the industry feel they unfairly target academic hospitals, which treat patients with more complex conditions and increased risk of developing HAIs (Hospital Acquired Infections), as well as hospitals that treat more low-income patients. The true intent of the penalties is to incentivize hospitals to continually focus on improving patient safety and quality. It is important to note, however, that of the 751 hospitals penalized for FY 2018, 425 were also penalized the previous year. Clearly, something needs to change.
Looking Towards the Future
While the penalties are not without fault, the program is expected to continue and hospitals will remain under scrutiny. So how do we work to improve overall patient safety and ensure penalized hospitals don’t become repeat offenders in 2019? In the midst of turmoil and uncertainty within the healthcare industry, increased CMS measures, and with a reduction in funding at stake, it’s never been more important to ensure your healthcare facility is utilizing a quality/risk management and performance improvement process that is both effective and efficient in mitigating, or even reversing, rising administrative overhead costs.
ActionCue CI provides capabilities for event reporting, quality management and performance improvement tracking in one easy-to-use online platform. It’s simple, collaborative and insightful, giving healthcare professionals access to real-time data that helps to streamline safety event reporting, while integrating it with quality and making performance improvement efforts much clearer and easier. This means your staff can not only quickly and efficiently document safety events, but also monitor the actions being taken to improve performance related to the area of concern. In 2018, Prista has worked with multiple healthcare organizations to document quality and safety improvements that have resulted in cost savings from $600,000 over the course of 10 months, to more than $1 million in prevented negative outcomes.
The system compiles and securely stores details on every adverse event, along with investigation procedures and findings, through a role-based workflow. With ActionCue’s clear and insightful visualizations, executives can easily view reporting and benchmarking, and tailor reports in minutes with just a few clicks. Our goal is not only to improve quality and performance management, but to ensure staff find day-to-day processes more efficient and enjoyable.
We value every effort hospitals are making to improve patient safety and overall quality of care. A safety penalty and subsequent reduction in funding is an unfortunate circumstance to say the least, but we’re here to help penalized hospitals bounce back and take the right step towards quality and performance improvement. If you’re interested in learning more about ActionCue, read what our clients have to say about the tool, check out our video library, or contact us today to discuss how we can work together to make a positive impact on patient care.

Increasing Efficiency in 2018
It’s the beginning of a new year, and in 2018 the healthcare industry would greatly benefit from better utilization of resources. U.S. health care spending grew 4.3 percent in 2016, reaching $3.3 trillion, while an estimated $1 trillion is wasted each year on inefficiencies, redundancies and abuse. With an aging population, and chronic illnesses and obesity on the rise, emergency department staff will continue to be flooded with patients, while hospitals work to comply with new CMS mandates and rulings, and improve quality of patient care.
Hospitals are constantly working to increase productivity and reduce expenditures, while statistics continue to remind us that time is money. In 2017, EY conducted an advisory study of the healthcare industry, and after analyzing the data, suggested a holistic approach to reducing inefficiencies and improving quality of care. Of the five points presented, we’ll focus on the three areas where our ActionCue CI platform can make a significant impact for healthcare organizations in 2018: transforming the culture, advancing with analytic insights, and increasing productivity
Transforming the Culture
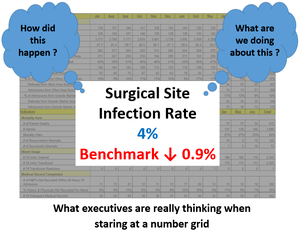
In 2017, we presented a four-part series on innovation and the role of leadership in creating action that improves patient safety and quality. A recurring theme in the series, and a concept we work to continuously promote, is creating a “culture of quality.” Improving culture is the first step towards improving patient safety and reducing inefficiency, and it must begin at the top. Organizational leadership must be deeply involved and aware of the challenges clinical staff face daily. Executive engagement is crucial to improving overall culture, but it’s no secret that executives face substantial time constraints. According to Becker’s Hospital Review, the average CEO spends about 2.5 hours per day in meetings, and 21.2% of a CEO’s solitary workday is devoted to reading and analyzing reports.
ActionCue CI allows staff to create comprehensive, easy-to-read reports in minutes, not days, providing real-time access to insights and performance measures while reducing time spent in meetings or analyzing confusing data sets. This creates more time for leadership to engage with clinical staff and take a more involved approach to culture. Because 51% of EY respondents believe employee satisfaction in healthcare drives patient satisfaction, not only will this boost morale, it will positively impact patient care.
Advancing with Analytic Insights
Access to reliable, accurate and insightful data is imperative as hospitals work to improve performance and quality. There’s more focus on patient outcomes than ever before, and as CMS continues to impose regulations and mandates, the spotlight is on hospitals to perform or risk losing funding. Executives need immediate access to meaningful metrics on safety events, corrective actions, performance indicators, quality management, risk management and more.
With event reporting, quality management and performance improvement tracking in one easy-to-use online platform, ActionCue CI is your Fast Path to Insight™. Its robust, real-time reporting features give executives the data they need to be proactive, rather than reactive, and drive better clinical outcomes.
Increasing Productivity
Organizations’ leaders have historically accepted that quality and safety efforts require a large amount of time and effort, and lengthy processes. However, we believe applications should focus on collaboration and workflows that not only match the natural tasks and processes of users, but also shape the users’ behavior by encouraging methodologies that produce targeted results, and increase efficiency and accountability.
ActionCue’s design goes beyond ease-of-use to advance the way in which healthcare organizations engage with information in an application. The platform proves to be an enjoyable working team member, increasing productivity and facilitating education and improvement towards goals. Executives hoping to cut costs in 2018 should place significant focus on improving productivity and efficiency. With low operation costs, no hardware or installation requirements, and month-to-month subscriptions, the impact of ActionCue CI on cost reductions is two-fold.
As the healthcare industry continues to place more emphasis on quality and performance improvement, and improved clinical outcomes, 2018 promises to be a year during which increased efficiency and better utilization of resources is a major focus, and rightly so. If you’d like to learn more about how ActionCue CI can help you reach your quality and performance improvement goals more efficiently, contact us today and start 2018 off on the right foot.

PDCA vs. OODA: Facilitating a More Effective Improvement Methodology
As we work to continually evolve Prista’s ActionCue Clinical Intelligence (CI) application as the leading performance improvement workbench in the healthcare market, we often dig into the essence and science of improvement itself. The ActionCue application not only embodies well-designed and powerful information processing, but also demonstrates an awareness of the principles and psychological aspects of improvement methodologies.
Since the application is designed around these fundamentals and not overtly focused on the mechanics of any particular methodology, ActionCue’s design can support a variety of improvement mentalities. One approach to improvement frequently used in circles outside healthcare is the “Observe, Orient, Decide, Act” (OODA) cycle illustrated above. Ultimately, OODA is comparable in process and effectiveness to the “Plan, Do, Check, Act” (PDCA) cycle, but is nuanced in ways that may be applicable and valuable for healthcare .
As widely understood and utilized as the PDCA cycle is, many people subliminally think of the cycle and its steps as always in process across a variety of projects or topics, which can help support continuous improvement. While such cycles are intended to be continuous, the application of PDCA often begins with a plan developed by trained experts, to study certain functions or performance measures, or experiment with a technique, practice or protocol. Unfortunately, time and resource constraints in healthcare quality and safety efforts frequently dictate that as one improvement plan is undertaken, another gets retired.
OODA begins when someone—in some cases an improvement specialist, but often an executive—observes something that needs to be improved. This makes the process seem more immediately reactive than PDCA, which explains the popularity of OODA in the military and construction industry, where unexpected challenges arise requiring critical and immediate attention. Although it’s helpful for those initiating any process to denote a starting point,
Consider an executive with responsibilities stretched across the entire organization. One of the biggest challenges for management and executives is shifting mental focus as different departments or activities require his or her attention. While some members of the clinical team or supervisory staff may easily engage with and understand a certain sets of metrics, collection of related safety events or performance improvement project, those who have to do more frequent and significant context shifting can benefit from additional explanation and illustration, and will often ask for the “big picture.”
ActionCue CI’s Performance Standard Dashboard presents that big picture, with easy-to-follow links to additional presentations of related data, information and insight. These data hierarchies are designed to match the cognitive pathways of a healthcare leader, providing what we like to call the Fast Path to Insight™. Gaining insight is a crucial part of the “Orient” step in OODA, and when done well and quickly, leads to more effective “Decide” and “Act” steps. An understanding of the executive mindset and management process, functional integration, easy-to-use navigation, intelligent design, and a foundation of analytics, all play a part in providing effective insight.
The design focused on cognitive pathways and support for OODA orientation are not just valuable for executives. All users of ActionCue CI, in a variety of roles and with differing responsibilities, enjoy enhanced efficiency and productivity in their work, largely due to integrating daily into intuitive workflows. This is applicable whether a user is oriented to the OODA or PDCA mindset. All users collaborate and engage with necessary information more easily and when using ActionCue CI, and that is a big win.
