Patient Safety is defined as “the absence of preventable harm to a patient and reduction of risk of unnecessary harm associated with health care to an acceptable minimum.” Every hospital in America has a stated mission to prioritize Patient Safety above all else. “First, do no harm” is the most fundamental principle of any health care service. Every healthcare organization says it, but are they really doing everything they can to prioritize patient safety?
The first step to solving a problem is admitting that you have one. But what if you aren’t aware that you have a problem? Especially in the Critical Access and Community Hospital space, where staff is stretched to non-optimal lengths, how can a facility, not only stay on top of patient safety, but take the time necessary to rigorously evaluate processes and policies to improve their quality of care?
Beyond the moral and ethical obligation to provide the best health care possible, there are clear financial benefits, although often unrecognized, unknown, or undervalued, to doing no harm. When was the last time you truly evaluated your facilities process of minimizing risk events, and optimizing quality outcomes? Could it be improved upon? Can it make your facility more profitable? The answer is a resounding yes.
Look at your patient fall data to see how much you’ve paid for Cost of Harm falls last year – what else could your hospital have used that money for? Next time you need to tighten your budget, remember cost cuts don’t just come from lowering staffing or standards. You can also save by minimizing how much quality and risk incidents are costing your hospital.
We’ve found this is true amongst our customers. Using ActionCue© CI’s Performance Improvement Plans and the guidance of our Implementation & Support team, one of our customer hospitals reduced falls at their facility by 25% over three years. Based on the Center of Disease Dynamic’s Cost of Harm figures, this saved them almost a million dollars in additional costs.
Another hospital saved more than a million dollars over three years as their CLASBI cases reduced by almost 47%. A third hospital saved more than $80,000 by cutting their rate of VAP cases by 66% in three years of using ActionCue CI.
Improving the quality of care, through proactively tracking and tackling risk and quality incidents can lead to significant savings from the cost of harm avoided – money that can fund additional staff, equipment upgrades and other improvements.
This positive cycle can multiply – every dollar saved by avoiding a Cost of Harm event can be spent on further eliminating Cost of Harm events, leading to more savings from the cost of harm avoided. As the cycle continues, avoidable costs decrease while the quality of care – and your reputation – increases.
This article first appeared in the March 2024 edition of Marketplace, the monthly newsletter of TORCH Management Services, Inc.

In his recent article “Leadership is Personal” published on LinkedIn’s Pulse, Keith Thurgood (also a member of Prista’s Board of Directors) notes that, “Despite spending billions on leadership development programs, [these programs] have not achieved their intended outcomes.”
Keith then goes on to say that “leadership is really about influence” and “Leaders understand that context, culture and collaboration matter when it comes to influence.” He then discusses the importance of self-awareness and how effective leaders must work on their personal development from the inside-out.
I always appreciate Keith’s insights, and reflecting on his article took me through ‘leadership’ as a thought exercise and into leadership as a learned set of behaviors – leadership becomes a habit, if you will. Some might call this ‘second nature’ because effective leaders make it appear so natural, but that’s not right, either.
By its very nature, leadership is not a solo practice. If leadership skills are not embodied in certain key collaborative work practices, their effectiveness will fade over time. What are those key collaborative practices, and how can they be facilitated?
At Prista, our experience with clients has made it very clear that the ongoing information work regarding the primary purposes and functions of an organization needs to directly serve the leadership function of that organization. This means the information work needs to deliver leveraged, actionable insights to leaders, not mass data, and these insights need to come from the work process itself, not from quarterly reports.
Leaders give direction and feedback that must be communicated directly and used in the collaborative process, not watered-down nor delayed by coming through side-channel briefings or bulletins. When this happens, real-time accountability becomes “built-in” to the way teams operate.
To be effective and efficient, the flow of information needs to leverage Information Technology and not be a massive human effort. Speaking of Healthcare IT design, Ted Melnick, Director of the Yale Clinical Informatics Fellowship, advised “Relentlessly question why things are done a certain way to ensure health IT doesn't get stuck in a cycle of ‘we do it this way because that’s how we've always done it.’”
Chris Coburn, Chief Innovation Officer at Mass General Brigham (Boston) had this to say about innovation: “Know your organization. Its people and culture will be the source, enablers and, at times, obstacles to innovation.” Leadership is personal, but leading requires a team and being an effective leader involves enabling the team’s success and removing obstacles.
In speaking about innovation teams at Houston Methodist, Michelle Stansbury, VP of Information Technology, takes steps to “ensure that we are focused on the right problems and we can quickly operationalize the transformational solutions.” That’s the key – it’s not information for information sake, or work for work sake, but rather developing solutions that lead to positive changes.
In other words, demanding, seeking and choosing fundamentally innovative design in the tools that equip the business is required, but so is end-user buy-in and participation. When this all comes together, leaders' relationship with information and its use in the organization changes dramatically to the benefit of all.
Prista’s ActionCue CI is an innovative, intuitive, easy-to-use platform that goes beyond traditional reporting to provide actionable insights in real-time. With ActionCue CI, information is more readily available, more meaningful, and more actionably insightful for healthcare executives, managers, and clinical staff. Contact us today if you’d like to learn more.

In March 2019, a Tennessee woman filed suit against Nashville-based Vanderbilt University Medical Center, claiming surgeons operated on her wrong kidney. As a result, the patient had to have a second surgery to correct the mistake, and she now needs dialysis for life. While this case was both rare and extreme, the fact remains that damaging medical errors are quite common, yet often preventable.
The World Health Organization (WHO) says more than 1 million patients die every year from surgical complications. And, there is a 1 in 300 chance of a patient being harmed during health care.
Clearly, more should be done to improve healthcare safety and quality and reduce risks to patients. Yet to say that the challenges of healthcare risk management are complex would be an understatement. Existing processes for risk management are fragmented and lack standardization. Many healthcare providers continue to use inferior systems that fail to analyze and synthesize data in a meaningful way. And all this in a rapid-fire environment, where threats can materialize in an instant.
Searching for the How and Why
When viewed as an individual benchmark, medical error reports only uncover so much. For example, an incident report of the Vanderbilt case would certainly show that the wrong site was operated on. But the more important question is Why? Perhaps the surgeon had been working too many consecutive hours. Maybe there was misinformation between departments. Or maybe a critical pre-op step, such as marking the operation site on the body, was overlooked. And if it was, why?
The how and why behind an incident are the real agents of change.
Finding the root causes behind errors in patient care is critical if we hope to prevent them from happening again. In fact, the only good that can come of such mistakes is the opportunity to learn from them and make process improvements – ultimately improving the standard of care and saving lives.
Risk Management Software for Increased Patient Safety
Reducing errors in patient care is not about having more medical knowledge, it’s about operational performance. And a basic incident report won’t change much.
When a safety event occurs, the first step is to record the basic facts in a patient’s medical record. While this step is both necessary and required, it excludes the information that is most important for analysis, learning, and operational change in the organization.
When things go wrong, both front line staff and healthcare administrators need access to comprehensive facts and circumstances surrounding the incident – as well as a clear, streamlined, and accountable improvement process. Fortunately, the right performance improvement platform can both identify and offer cues towards effective corrective and preventative actions, or CAPAs.
Hospitals, regional clinics, and surgery centers will benefit greatly from a single, comprehensive system for risk management., particularly one that integrates the many performance measures across the board, and that integrates all these activities into a goal-oriented, coherent whole. In order to keep up with the pace of care, they need analysis and synthesis of data in real-time. And most importantly, they need clear and manageable action plans based on that analysis.
The right platform for quality-safety improvement can provide insight into past incidents, identify existing performance trends, and offer a view of the future. ActionCue CI’s comprehensive dashboard facilitates the collection of information and circumstances surrounding healthcare incidents including planning errors, process errors, and failures to act.
Here are some of the key ways ActionCue CI makes quality-safety tracking and improvement more effective:
- Anyone on staff can originate an Event Report with little or no training
- There are 26 categories of events covered including Complaints/Grievances, HIPAA incidents, Abuse, Plant/Facility, Readmission, Sentinel Events, Security and Work-related Injury
- The distributed workflow not only distributes the workload but obtains inputs from the best people to do so, including those nearest to the time and place of the event
- Event Reports are passed to the next person in the workflow based on roles, permissions and assigned parts of the organization
- The workflow, appearance and experience are designed with expertise in several disciplines
- Individuals or groups have assigned responsibility for each step, but others can observe and review the content, or can be requested to confer on the content
- Workflow progress is tracked so that stalled reports are identified to managers who can send reminders
- Content (documents, photos, videos)can be uploaded/attached to the Event Report at any stage
- Alerts can be immediately sent to select individuals when content of designatedcriteria is saved
- Those with permission can track, review and research the Event Reports using a range of content filters while they are in progress or after completion
- Follow-up activities, beyond the primary track of the Event Report workflow, can be tracked in terms of scheduled reminders and information or documents exchanged, with any internal or external organization
- Built-in analytics and reports provide distribution data (histograms) of content occurrences, weighted analyses, time spent by workflow stage and event category, and much more insight, as soonas the events Reports are finalized, without any time delay or human effort.
- Certain facts and circumstances are tallied in the Event Reports to form data points used in numerous Performance Measures like Fall Rate, Medication Variance Severity, and many more
- Event Reports can be linked to Performance Improvement Action Plans, and vice versa, for easy human analysis
While some of these features may be of particular interest or importance to various users, the real power of ActionCue CI is that it was designed for a specific purpose – facilitating all stakeholders having a fundamentally different relationship with the data that allows them to better leverage their time and energy for true improvement. While the change-averse may initially balk at such a dramatic shift, it is the right approach for long-term gains throughout the organization. Optimal gains can only be achieved through a platform designed for this purpose.
Mistakes in healthcare have bad consequences for everyone, from injured patients to physicians who may face legal and professional troubles. By working to eliminate medical missteps, healthcare professionals can protect patients and themselves while lowering operational and cost inefficiencies in delivering better care. But if institutional practices do not change, nothing will change.

When it comes to discussions about healthcare reimbursement and costs, “Value-Based Purchasing” is a term that gets thrown around quite a bit these days. In fact, many experts say it’s going to be the future for healthcare organizations.
Due to its growing use in hospitals and regional clinics, Value-Based Purchasing (VBP) has become a buzzword in healthcare. But as often happens with buzzwords, the original meaning becomes less salient to most people than their feelings and experiences with the subject. What exactly is the goal of value-based purchasing?
The Goal of Value-Based Purchasing
On paper, the methodology of VBP is simple: pay providers for quality and value, not just volume. Hold healthcare organizations accountable for both the quality and cost of the care they deliver and reward the best-performing providers.
The goal of VBP is to facilitate a high-level of care that is both safe and efficient. To reduce medical errors, lower the rate of accidents, achieve better patient outcomes, and maximize financial rewards. In an ideal world, clinics and hospitals will operate at optimal effectiveness and efficiency – resulting in lower prices for both patient and payor.
The Reality of Value-Based Purchasing
Organizations work hard, month after month, to achieve this noble “value proposition”. But the everyday reality of succeeding for their organization in a Value-Based Purchasing program is far from simple.
Value-based care goals come with their own elaborate set of rules, metrics, benchmarks, reimbursement adjustment tables, and a million other things. The delay between capturing data and applying benchmarks to a provider’s reimbursement is significant. It’s all too easy for care providers to become immersed in the administrative minutiae of VBP and lose track of the program’s highest goal – better value for patients.
Therefore, whether you’re a front-line staffer or a top-level executive, it’s important to circle back to one basic question: “Does what we’re doing truly improve value?”. If the answer is “No” or, (as is often the case), unclear – then it’s time to evaluate the effectiveness of the task, process or tool on a fundamental level.
Getting Back to the Value in VBP
In order to shift the focus back to “value” in a value-based purchasing system, major changes need to occur in how departments think and work together.
Of course, a VBP-participating provider organization cannot completely ignore the necessary mechanics of the program without losing the reimbursement boosts it can provide. However, when the staff and management can focus on actual performance across the majority of their care-delivery operation, on a real-time basis, VBP success becomes a byproduct of genuinely improved clinical performance across the board.
As we see it, there are some real opportunities for core value improvement in the fundamental way the quality improvement operation is executed. For example:
- Change the focus from reporting to insight, learning, and change. Lengthy and detailed reports do not improve anything. Make the improvement process the primary core function, make it effective and efficient, and reverse engineer the way the capture, processing, communication, and work on that related information is built to optimize improvement in Quality and Safety.
- Involve executives by giving them the right lens on the subject matter. ActionCue’s event reports capture the facts and circumstances surrounding each adverse event, while the performance measures and analytics capture a big, coherent picture of the operations. Only by replacing the “too many moving parts” nature of Quality-safety with a complete story can we hope to provide proper executive buy-in and leaders to improve evidence-based outcomes and quality measures.
- Get away from paper as inputs or outputs. Paper is static information that takes human effort to move, change and work on. ActionCue CI gives uses a workbench to support information work and receive actionable insights in a dynamic way.
- Don’t be afraid to re-invent the process. Stop throwing more human effort at things that aren’t getting results, just because it’s “the way we’ve always done it.” That includes classes and meetings, that soon fade and impact the work far less than equipping the staff to actually work differently.
- Think outside the box. The “mandated” way is not always the best way! Don’t let a mandated task, step or artifact chain the organization to an outdated, suboptimal overall process. Look for new and fundamentally more efficient processes that serve goal attainment, even if those small mandated tasks, that deliver less value, seem redundant.
Remember, the most precious things your team produces in running your operation and delivering care are actionable insights to improving value. If you’re working more and getting less of that, CHANGE. Because the goal, after all, is value. Value for patients and value for care providers.
Healthcare has too many moving parts. It’s a common cry in the industry, especially for healthcare quality and safety professionals.
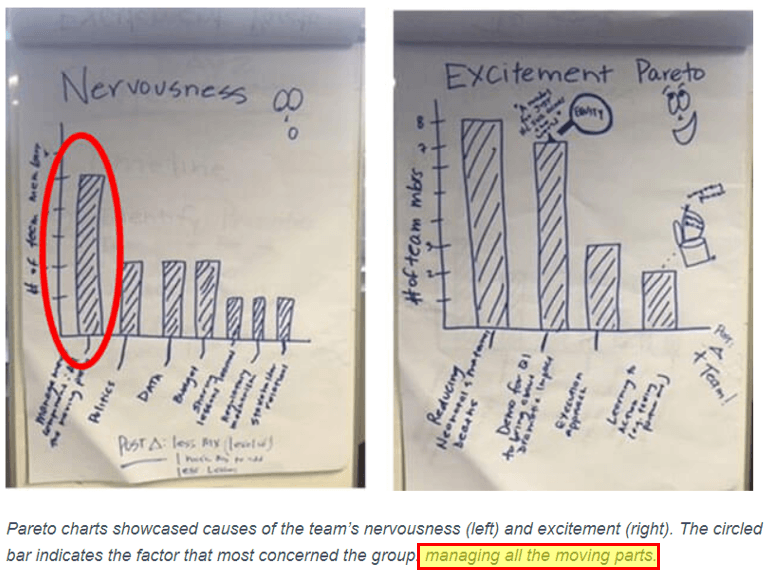
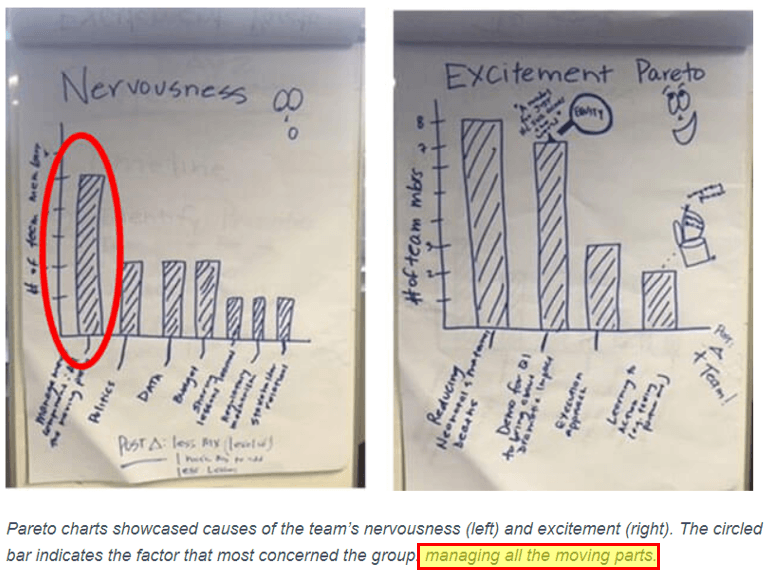
In January 2019, the Institute for Healthcare Improvement (IHI) polled a group of members embarking on a large-scale project to reduce maternal and newborn mortality. When asked what aspects of the project made them most nervous and what made them most excited, “managing all the moving parts” was the top cause of concern.
As the poll indicates, between reporting, forms, metrics and insurance, plus the innate complexities of patient care – things can get complicated very quickly.
The Challenge: Too Many Moving Parts
The “moving parts” dilemma is all too familiar to healthcare quality and safety professionals. When it comes to patient care and process improvement, it’s always been a delicate balance between quality, safety, and context.
Too often, there exists a large gap between “ticking the box” and the actual process of conceiving, planning and evaluating improvements. When metrics and event reporting become mutually exclusive tasks within healthcare organizations, everyone suffers. Departments miss out on the benefit of shared information, and the level of patient care remains stagnant or worse, declines.
There are a few healthcare IT products on the market that aim to tackle the moving parts problem – but most of them fall short. You find yourself manually moving and processing data or repeating tasks because system modules don’t “talk to each other”. Simple calculations are left to the user. Navigation of the application is overly complex and language unintuitive. Users’ engagement with the various systems and methodologically-driven manual processes is daunting and painful.
Healthcare organizations are looking for the most efficient ways to leverage human, financial, and physical resources in support of top-notch patient care. Despite best efforts though, non-universal systems & software, and information silos between departments often get in the way of progress. The result is a lot of fractured effort and reduced productivity.
The Solution: Informed Insights, Action Plans
What if you could spend less time managing “moving parts” and more time providing and improving patient care?
What hospitals need most are healthcare technologies that not only collect data, but also provide context and insights that lead to better and safer patient experiences. They need software solutions that are easy-to-use, intuitive, collaborative and, most of all, coherent.
Quality performance metrics matter, but they don’t tell the whole story. Metrics force you to work with simple data, while what you really need are the actionable insights derived from that data. And, managers and executives trying to drive improvement need answers to “How did we get here ?” and “What are we doing to fix this ?” without going on a safari or waiting on an analyst or staffer to chase and manufacture those answers.
Our number one goal behind the design of ActionCue CI was smoothly bringing together all those “moving parts”. Separate functions and departments for Quality Management, Event Reporting and Performance improvement don’t reflect, and don’t contribute well to, the true, unified goal of optimizing patient care and its costs. More than just another set of spreadsheets, event reporting software, and assembled briefing book – metrics, facts and progress tracking are synthesized into valuable insights with corresponding cues. The innovative new technology supports patient-centered care by facilitating management and work for performance improvement projects. One Goal. One Platform. Coherent Insight.